Nursing diagnosis for diabetes insipidus plays a crucial role in guiding patient care and ensuring optimal outcomes. This condition, characterized by excessive thirst and urination, requires a thorough understanding of its pathophysiology, signs, and symptoms to facilitate accurate diagnosis and effective management.
Diabetes insipidus encompasses various types, each with distinct etiologies and clinical presentations. Central diabetes insipidus, resulting from inadequate antidiuretic hormone secretion, and nephrogenic diabetes insipidus, caused by impaired renal response to antidiuretic hormone, are the primary forms. Understanding these variations is essential for developing individualized care plans.
Overview of Diabetes Insipidus
Diabetes insipidus is a rare condition that causes excessive thirst and frequent urination. It is caused by a deficiency of antidiuretic hormone (ADH), which is a hormone that helps the kidneys reabsorb water.
There are two main types of diabetes insipidus: central diabetes insipidus and nephrogenic diabetes insipidus. Central diabetes insipidus is caused by a deficiency of ADH, while nephrogenic diabetes insipidus is caused by the kidneys’ inability to respond to ADH.
The signs and symptoms of diabetes insipidus include:
- Excessive thirst
- Frequent urination
- Dilute urine
- Dry mouth
- Constipation
- Fatigue
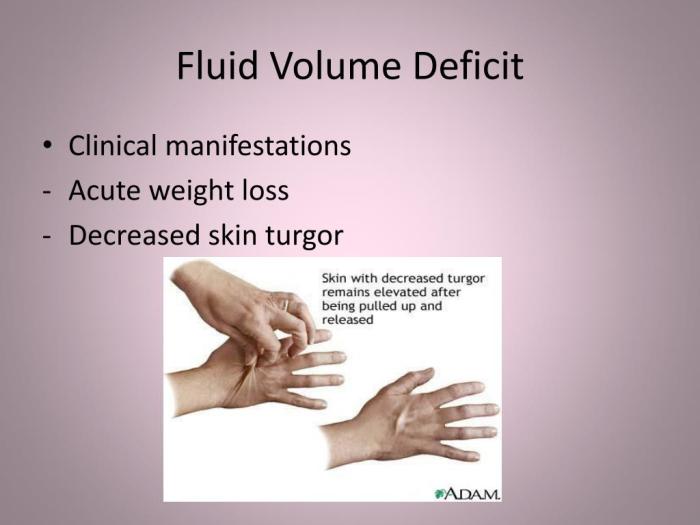
- Weight loss
Nursing Diagnosis for Diabetes Insipidus
The nursing diagnosis for diabetes insipidus is:
Deficient fluid volume related to impaired renal water reabsorption
The defining characteristics of this nursing diagnosis include:
- Excessive thirst
- Frequent urination
- Dilute urine
- Dry mouth
- Constipation
- Fatigue
- Weight loss
The related factors that contribute to this nursing diagnosis include:
- Deficiency of antidiuretic hormone (ADH)
- Inability of the kidneys to respond to ADH
Nursing Interventions for Diabetes Insipidus: Nursing Diagnosis For Diabetes Insipidus
The nursing interventions for diabetes insipidus include:
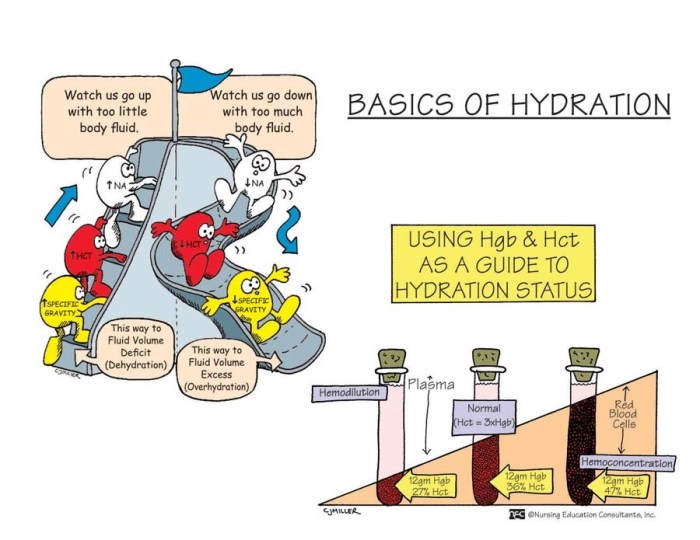
- Monitor the patient’s fluid intake and output
- Encourage the patient to drink plenty of fluids
- Administer medications to increase ADH levels
- Protect the patient from dehydration
- Educate the patient about the condition and its management
The rationale for these nursing interventions is as follows:
- Monitoring the patient’s fluid intake and output helps to assess the patient’s fluid status and to identify any fluid imbalances.
- Encouraging the patient to drink plenty of fluids helps to prevent dehydration.
- Administering medications to increase ADH levels helps to improve the patient’s ability to reabsorb water.
- Protecting the patient from dehydration helps to prevent complications such as seizures and coma.
- Educating the patient about the condition and its management helps the patient to understand the condition and to make lifestyle changes to manage the condition.
The expected outcomes of these nursing interventions include:
- The patient will maintain a normal fluid balance.
- The patient will be free of dehydration.
- The patient will understand the condition and its management.
Evaluation of Nursing Interventions
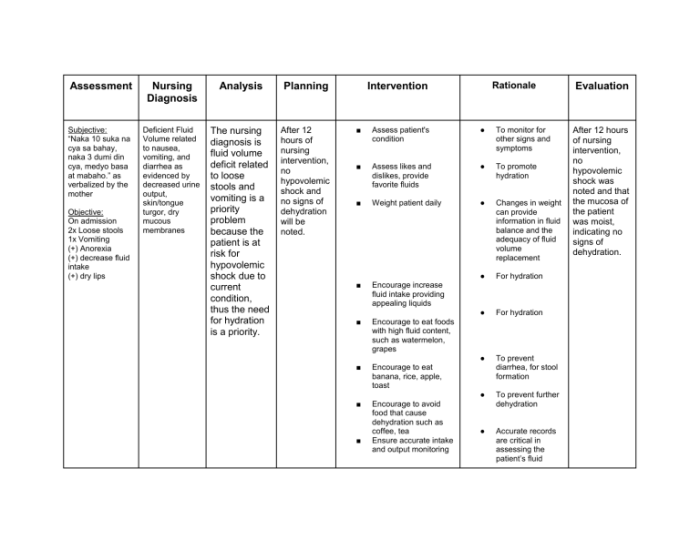
The effectiveness of nursing interventions for diabetes insipidus can be evaluated by assessing the patient’s fluid balance, hydration status, and understanding of the condition and its management.
Indicators that demonstrate successful outcomes include:
- The patient’s fluid intake and output are balanced.
- The patient is free of dehydration.
- The patient understands the condition and its management.
Challenges in evaluating nursing interventions for diabetes insipidus include:
- The patient’s fluid intake and output can be difficult to measure accurately.
- The patient’s hydration status can be difficult to assess.
- The patient’s understanding of the condition and its management can be difficult to evaluate.
Case Study
A 55-year-old male presents to the clinic with a history of excessive thirst and frequent urination. He has been experiencing these symptoms for the past several months. He has also lost 10 pounds in the past 6 months.
The patient’s physical examination is unremarkable. His blood pressure is 120/80 mmHg, and his heart rate is 80 beats per minute. His urine output is 5 liters per day, and his urine specific gravity is 1.001.
The patient’s laboratory tests show a serum sodium level of 145 mEq/L, a serum potassium level of 4.0 mEq/L, and a serum creatinine level of 1.0 mg/dL.
The patient is diagnosed with diabetes insipidus.
The patient is started on a treatment plan that includes:
- Monitoring his fluid intake and output
- Encouraging him to drink plenty of fluids
- Administering desmopressin acetate (DDAVP) to increase his ADH levels
- Educating him about the condition and its management
The patient’s symptoms improve significantly after starting treatment. He is able to maintain a normal fluid balance, and he is no longer experiencing excessive thirst or frequent urination.
Expert Answers
What are the common signs and symptoms of diabetes insipidus?
Excessive thirst, frequent urination, dehydration, fatigue, and weight loss.
What is the primary nursing intervention for central diabetes insipidus?
Administering synthetic antidiuretic hormone to replace the deficient hormone.
How is nephrogenic diabetes insipidus managed?
Treatment focuses on managing symptoms, such as fluid replacement and medications to reduce urine output.